Obstructive Sleep Apnea:
The Definitive Guide
Introduction
Do you ever ponder about your breathing or sleep?
Usually not, right? Because these are automatic activities for someone in good health.
But if you belong to the 18 million Americans suffering from sleep apnea, according to the National Sleep Foundation, then you probably do.
The term apnea describes breathing pauses of ten seconds or more.
Sleep apnea is an ever-increasing issue in modern society.
Can you think why?
If you thought obesity and overweight, then you guessed right.
The medical community recognizes that there is a clear link between excess weight and sleep apnea.
The stereotype snorer, in comedy routines and silly cartoons, is someone overweight with a short and sturdy neck.
And may I hazard a guess? You are probably thinking that if this overweight, sturdy neck person snores very loudly, then he is likely an apneic patient.
This may not be true though, and obstructive sleep apnea (OSA) can also affect thin people who do not snore.
So, you should feel concerned, whether you do or do not have the “physique du role”, especially if you often feel drowsy during the day.
And this is because daytime sleepiness is not the only consequence of obstructive sleep apnea (OSA).
A study over 18 years, in 1522 individuals from the general population, reported some shocking results.
People with severe, untreated sleep-disordered breathing died 3.8 times more often than those without.
And these results, while alarming, may not be so surprising after all.
Untreated OSA deprives your brain, organs, and tissues of oxygen as you sleep.
Yes, oxygen! Nothing else!
No wonder, so many serious health effects are associated with OSA.
The decreased blood oxygen levels can affect how some internal organs’ function. They can also worsen other pathologies.
Read on to understand OSA, as well as the consequences of oxygen deprivation and fragmented sleep on your body.
Of snoring and sleep apnea
What is snoring?
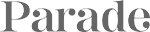
When you rest at night, your uvula and soft palate tissue relax, become flabby and lose their tone.
Because of your horizontal position, gravity pushes them against the rear part of the mouth, along with your tongue.
Your snoring results from the vibration of your soft tissues:
- uvula,
- soft palate,
- pharynx,
as you inhale air, like sails flapping in the wind.
How frequent is snoring?
According to the American Academy of Otolaryngology-Head and Neck Surgery, your chance of being a habitual snorer is 25% percent.
Interesting fact: this number goes up to 45% if one also includes occasional snorers.
And if you have children, then consider that 10% of them snore regularly.
But what about its impact on your health? … Read on to find out.
Is snoring a health issue?
Good news…
….. it is not a health issue per se and rarely does it occur with sleep pauses.
So, when should you seek medical advice?
If your sleeping shows alternate periods of snoring and moments of silence lasting a few seconds up to a minute where you stop breathing.
Then you may be suffering from sleep apnea, and if you do, your health may be affected.
The louder the snoring, the higher the chances that you may suffer from sleep apnea.
Check the next sections to learn about sleep apnea.
Is snoring the same as sleep apnea?
Nope, they are different.
And that’s true, despite the loud snoring of most people with obstructive sleep apnea (OSA).
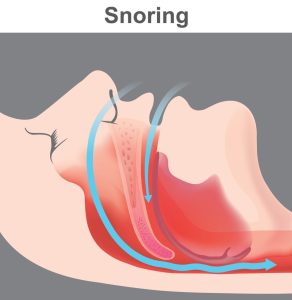
Sleep apnea consists in an obstruction of your upper respiratory airways. This can be either complete or partial.
And obstruction implies breathing efforts!
In other words, your body will start struggling to maintain the airflow. This will be either absent or significantly reduced.
As explained above, snoring instead can happen without sleep apnea.
Your snore could be loud even without any obstruction.
So, do not confuse the two!
How many types of sleep apneas are there?
The most common form is Obstructive Sleep Apnea (OSA). Hence, throughout this web site, we will use the term “sleep apnea” to refer to OSA.
However, there exist two other forms, albeit less frequent, called central or mixed apnea.
Let’s take a closer look at their different characteristics.
What is obstructive sleep apnea (OSA)
OSA is a sleep disorder where you have involuntary breathing difficulties that disturb sleep.
Apnea means “no breathing.”
Yes, nothing else!
Just by judging from its name you know it is a serious disease.
OSA is an ongoing condition (chronic) where you suffer from an abnormal high number of:
- reductions of respiration (shallow breaths) also called hypopneas,
- repeated interruptions of breathing during your sleep (hence the name “apnea”),
that occur during your sleep.
Muscles always relax when you fall asleep.
But as a sleep apnea patient, this leads to your soft palate narrowing or blocking of the airways at the back of your mouth.
During your sleep, this repetitive process causes:
- a partial decrease in airflow (hypopnea)
- or a complete airflow cessation.
Also, it will invariably lead you to snore more loudly, and even make choking sounds as you attempt to breathe.
Interesting facts:
- These breathing pauses last 10 to 30 seconds or more … even 1 minute!
- They can happen hundreds of times a night despite your breathing efforts.
And so, if you are guessing that your sleep will be lousy … well, you guessed correctly!
You will indeed suffer from poor quality sleep because of repeated short sleep disruptions.
Because of shallow breathing or breathing interruptions, you will repeatedly switch from deep into a light sleep.
The quality of your sleep will plummet.
Throughout the night, you will awake partially to resume breathing.
You may find yourself with:
- your heart beating faster,
- sitting in your bed,
- making an effort to free your upper airways.
Your respiratory reductions or interruptions will cause a lack of oxygen. This will lead your brain to trigger a reaction to overcome the problem.
The breathing pauses, and shallow breaths will generate sudden drops in your blood oxygen concentration. This could be down to 40% if you suffer from severe OSA.
Also, surprising fact, you usually won’t recall the events on the following morning.
Why?
Because you were usually not fully awake.
But, you will not feel refreshed and rested because of the repeated sleep interruptions throughout your sleep cycle.
As you may be surmising already, this will impact your daily life and health.
Check the next sections to discover how.
What are the likely consequences of OSA on your daytime activities?
It is unfortunate, but it is a fact: OSA will significantly affect your daily life.
Poor quality sleep will make you doze off during the day. You will struggle to concentrate, losing out on efficiency.
At times, you will also be unable to avoid falling asleep.
Your risk of having car accidents will also be seven times higher versus those who do not suffer from OSA (see Does OSA increase the chance of a motor vehicle accident? if you want to learn more).
Hence, it is important to understand how severe your OSA is.
But how do doctors assess its severity?
Jump to the next section for the answer.
What is the apnea-hypopnea index (AHI)?
It is a score used to assess the severity of your obstructive sleep apnea.
It captures:
- the number of apneas or hypopneas (also called partial apneas or shallow breaths),
- during 1 hour of sleep,
- measured via a polysomnographic machine.
The results are expressed via an index called apnea-hypopnea index [AHI].
And it is quite useful.
Do you know why?
Doctors will use this index to assess the severity of your disease.
For instance, the American Academy of Sleep Medicine states that you will be diagnosed with OSA provided some criteria are met.
And these criteria include your AHI.
To be diagnosed with OSA, your apneas, hypopneas (and sleep-interruptions with breathing efforts), must be:
- at least equal to 15 events/hour,
- or at least equal to 5 events/hour provided they occur at the same time as certain symptoms.
Doctors must use a polysomnographic machine to measure these events.

The criteria referred to above, also include:
- falling asleep against your will during times when you are awake,
- daytime sleepiness,
- waking up with choking or suffocation sensations,
- insomnia,
- description (e.g., by one’s spouse or partner) of significant snoring or breathing interruptions during sleep,
- tiredness.
The severity of OSA depends on the measurement of the combined number of apneas and hypopneas per hour of sleep. This is also referred to as the apnea-hypopnea index (AHI), if:
- AHI is between 5 and 15, then obstructive sleep apnea is mild;
- AHI is between 15 and 30, then it is moderate;
- if AHI > 30, then apnea will be severe.
Let’s now talk about the less frequent types of sleep apnea.
How do central, mixed or OSA differ?
As explained above, during OSA, your respiratory tract will collapse or get blocked during your sleep.
This slows down or interrupts breathing.
When you try to breathe, the air flowing through the obstruction will cause you to snore.
But how does central apnea differ?
Well, central sleep apnea is caused by a nervous system dysfunction. So, it is very different from OSA.
The area of the brain controlling breathing will transiently stop functioning. It will cease sending the correct nervous signals to the muscles in charge of your breathing.
Hence your body “will forget” to breathe during some very short instances.
If you suffer from central apnea, your pauses in breathing will occur without any effort to breathe.
Now, your likelihood of suffering from central apnea will increase if you:
- suffer from certain pathologies like cardiac insufficiency, stroke, and renal insufficiency,
- and if you take certain medications.
If you have central apnea, you will not suffer from frequent, ongoing snoring.
Why?
Simple! Because there is no airflow whatsoever.
Pure central apneas are rare.
OSA most often accompanies them, hence the term mixed apnea.
We said that pure central apnea is rare, but how frequent is OSA?
You will find the answer in the next section.
How frequent is OSA amongst adults?
To begin with, here is an interesting fact: out of 10 people suffering from apnea, 9 actually suffer from OSA.
You understood correctly.
OSA is much, much more frequent than all other apneas.
Reason why, during the rest of this article, we will focus on OSA.
But how many individuals does OSA affect in the population at large?
According to a recent source, those with moderate to severe OSA (with an apnea-hypopnea index ≥15 events/hour) are
- 10% among 30-49-year-old men;
- 17% among 50-70-year-old men;
- 3% of 30-49-year-old women;
- and 9% among 50-70-year-old women.
The statistics speak for themselves.
They show with clarity that it is more frequent in men and in older age groups.
And these numbers are higher among obese subjects.
A surprising fact is the underdiagnosis of the majority of OSA sufferers!
The findings from a 1997 study are revealing.
These showed that8:
- out of a sample of approximately 5000 patients employed adults,
- 93% of women and 82% of men with moderate to severe sleep apnea
- had not been clinically diagnosed.
This is probably because:
- no blood tests exist to diagnose sleep apnea,
- and it is not easy for your general practitioner to detect it during regular medical check-ups.
We have seen the statistics for adults, but what about children?
Next …
How frequent is OSA amongst children?
Luckily, little patients are less affected than adults.
1%-4% of this population suffers from the disease.
But OSA is more frequent amongst boys than girls.
Is OSA observed irrespective of age, within this young population?
Nope. OSA is more frequent among 2-8 years old children, and 12-16 years old adolescents.
But it affects all ages somehow. All the way from few-month-old babies to 18 years-old young adults.
Obstructive sleep apnea (OSA): signs, symptoms, risk factors and health impact
Are you at risk of developing sleep apnea? What are the risk factors?
Quick question: what are some of the characteristics, easy to identify, that will quickly let you gauge whether you are at risk for OSA?
…. Increased waist circumference and a large and short neck.
A short neck will tend to have a reduced airway passage.
And as for its size, it depends on your gender:
- if you are a man with a circumference of 17 inches (43 cm) or more, then your airways will be narrower;
- if, instead, you are a woman, a neck circumference of 16 inches (40 cm) or more you will make you more likely to present OSA.
Another neck related risk factor is excessive skin between your chin and neck. This is also known as turkey neck.

But, really, anybody can suffer from OSA.
Let’s now look at the rather long list of risk factors. These may interfere with the smooth functioning of your upper respiratory tract:
- If you are overweight or obese, your chances of presenting OSA will increase.
Why is that you may wonder?
Because the deposits of fat down the back of your throat, around the neck or chin.
These increase if you are obese, and they will tend to obstruct your breathing.
Obesity is considered the most important risk factor.
Even a modest weight loss can improve the quality of your sleep.
If you are obese or overweight, you have 50% chances of suffering from sleep apnea.
But there also many thin people presenting this syndrome, because they may have other risk factors – see below. - Gender: if you are a male, your chances of presenting OSA are also higher. And even more so if you are older than 40.
If you are a woman instead, the risk of suffering from sleep apnea will be half that of a man.
Now, what happens with age?
Well, this difference will decrease.
During menopause the ratio will be almost the same: “Disordered breathing during sleep is more common among postmenopausal women than among their premenopausal counterparts. … This is possibly due to the decline of levels of estrogen and progesterone.” - As we have just seen, Age is also a factor irrespective of your gender.
OSA is much more frequent in a population aged between 45 and 64 years.
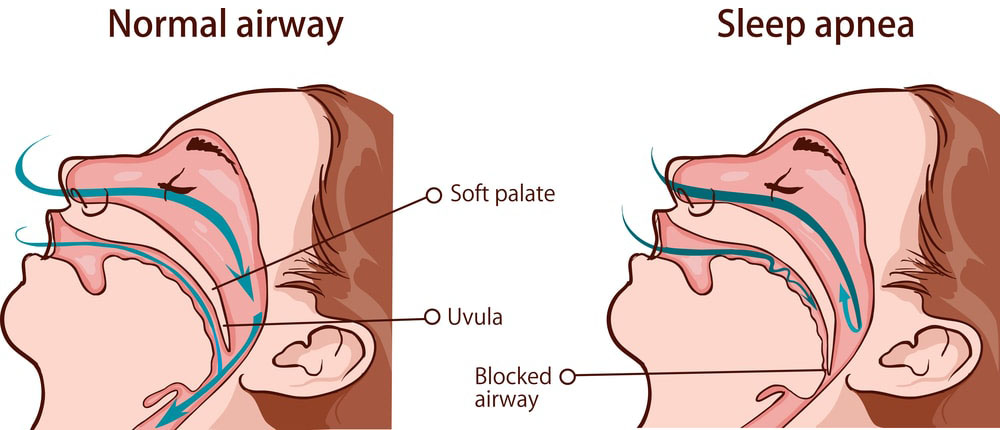
The risk further increases as you get older. - A family history of OSA or snoring will also increase your risk of suffering from the same syndrome.
Yes, there is a hereditary component for OSA!Unique genetic features determine the size and position of:- your jaw
- tongue,
- soft palate,
- tonsils,
- or uvula (see below image).
- Your ethnic group will also play a role. Asians and Afro-Americans have a higher risk of sleep apnea
- It is obvious that obstructions can also have an impact. These can be due to:
- diseases of ear, nose, and throat (otorhinolaryngologic disease),allergies,past surgeries.
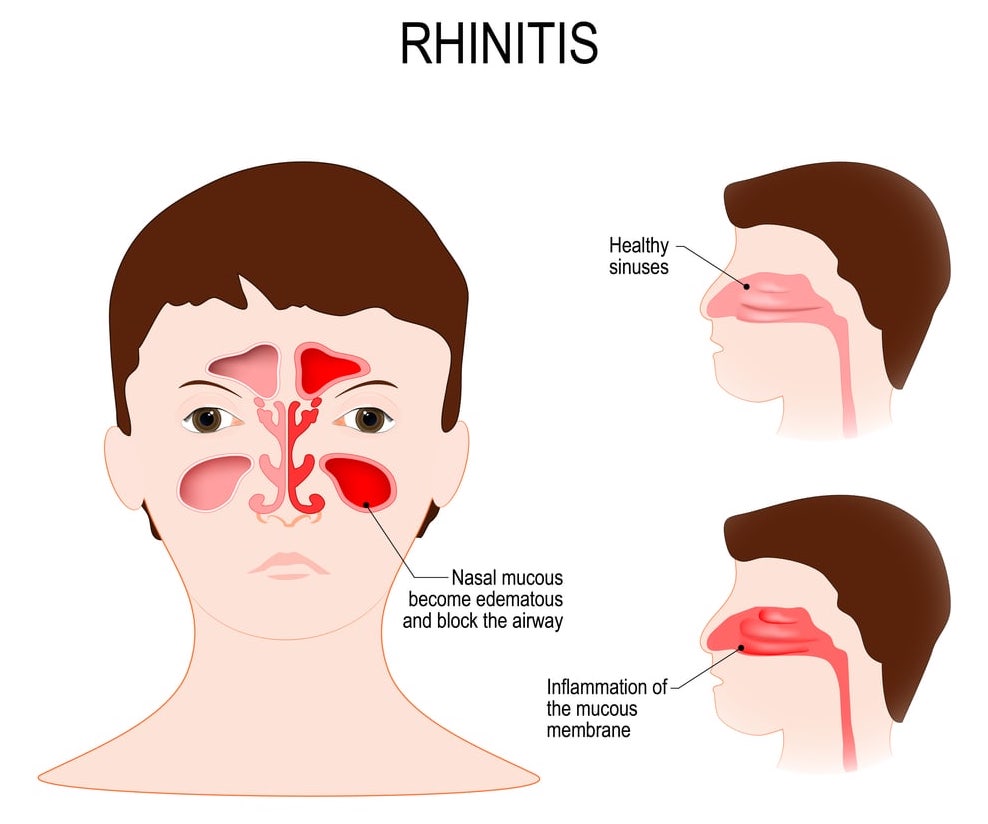
For instance, a study showed that if you suffer from allergic rhinitis, then this will influence your OSA.
OSAs will be longer and more frequent during a period of significant nasal obstruction than when symptoms are absent.
Results suggest that a high nasal resistance may influence the development of OSA (pathogenesis of OSA). - Sleeping with the mouth open is a sign.
Are you surprised? Well, you should not.
It is a sign of obstruction of the nasal airway.
Nasal obstruction causes the jaw to drop. This reduces the diameter of your pharyngeal airway. As a result, your likelihood of presenting OSA will increase.
Take this piece of advice: check with your family or bed partner if you are a sleeping mouth breather.
You may indeed be suffering from OSA. - Substances causing relaxation of your throat’s muscles, such as:
- alcohol consumption,
- sedatives,
- anti-anxiety medications,
- sleeping pills
- Smoking If you are a smoker and you ascribe your OSA to be due to something else, then think twice! Because smoking also plays a role.
You will be at higher risk for sleep-disordered breathing than if you do not smoke or if you have quit.
Smoking increases your likelihood to suffer from OSA by a factor of 2.5 or 3 versus non-smokers.
This may be due to an inflammation of the airways as well as fluid retention. They lead to a reduction of the volume available for smooth flow through the airways. - You suffer from diabetes type 2 you are at risk for OSA.
But if you expect a clear explanation, then you will be disappointed.
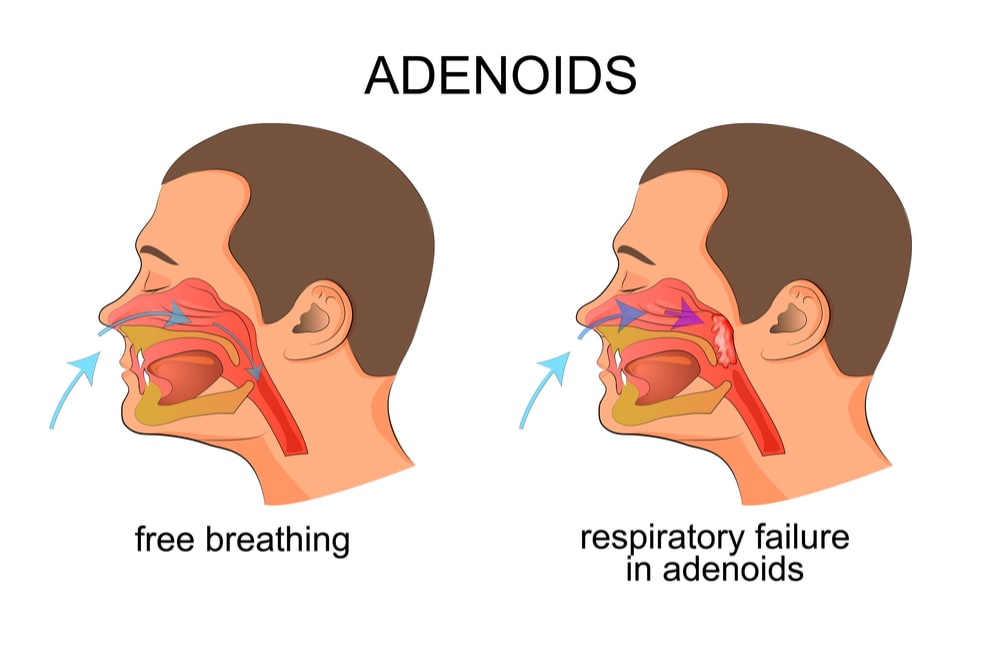
The reasons are not well understood yet, but obesity most likely plays a role. - Last but not least, enlarged tonsils and adenoids are also a risk factor for OSA…. And, you may have already guessed the reason … decreased airways passage.
For instance, an undersized lower jaw (versus the upper jaw) is a risk factor that may lead to OSA.A small lower jaw will remain in a posterior position, and the upper respiratory airway will be narrower.
This leads us nicely onto the next section.
What are the risk factors of developing OSA for your children?
Enlarged tonsils or adenoids are the most frequent causes in a pediatric population.
As their size increases, the flow through the respiratory airways becomes more difficult.
But the good news for your children is that airflow can resume after removal of these tissues.
It is the best option to solve the problem, and the surgical procedure is quite standard.
Other risk factors for your children include:
- obesity or being overweight,
- a narrow face shape.
We have looked at the risk factors for OSA, but what about symptoms and signs?
You just need to read on to find out.
What are the symptoms and signs of OSA in adults?
Surely, you should be able to tell with ease if you have OSA … right?
…. Wrong!
Your relatives or your bed partner are usually the ones who can help you do so.
You will probably not realize you have breathing difficulties during your sleep unless you identify the symptoms.
The same goes for gauging how severe your sleep apnea is.
And, when it comes to symptoms, you can divide them into 2 groups: major and minor.
Major symptoms
The main one is frequent and loud snoring.
It is the most common symptom occurring in 70% to 95% of patients.
You may stop breathing during sleep. These pauses may interrupt your snoring. After the pauses, you may be panting or gasping for air.
When you sleep on your back, the pressure on your respiratory airways will be more important than if you sleep on your side.

Hence, sleeping in a fetal position (on the side) will make your snoring less loud.
But, it cannot end your snoring if this was initially loud.
Will you snore every night?
Nope. Though it is likely that, with time, your snoring will gradually worsen and increase both in frequency and intensity (louder).
Another major sign of OSA is fatigue and feeling sleepy during your daily activities (work, travelling, etc.).
You will also find yourself struggling to avoid falling asleep during quiet times of the day.
Interesting facts:
- Drowsiness will permeate and increase during the day while taking a nap will usually be of no relief.
- You may even wake up more tired after a nap if apneic events interrupt it.
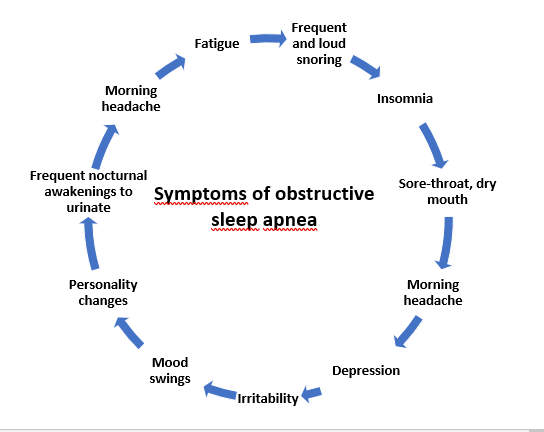
Minor signs and symptoms include:
- a morning headache,
- memory or learning problems,
- struggling to concentrate,
- irritability,
- depression,
- mood swings,
- personality changes,
- frequent nocturnal awakenings to urinate,
- (as you wake up) sore-throat or dry mouth,
- drowsiness and uncontrolled daytime sleepiness when you work or drive.
Let’s now see what the symptoms are in a younger population.
What are the symptoms and signs of OSA in children?
Little patients have somewhat different symptoms than adults.
Unlike them, they do not show sleepiness. Instead, they display restlessness and overactive reflexes.
As a parent you will also observe behavioral disorders that characterize a “real problem child” like:
- hostile or angry behavior,
- sudden mood change,
- a tendency to cry easily.
Other issues will be present like:
- Lack of attention at school, and poor school performance,
- a tendency to breathe through their mouths (instead of their noses) during the day,
- struggling to remember things they learned at school.
On the good side though, you will not have to worry about:
- cardiovascular complications such as high blood pressure,
- and excessive weight gain.
Final remarks
If you think you have read enough, and you are looking for a sleep apnea dentist in New York, then look no further! Book an appointment with us now.
Otherwise, since we broached the subject of health effects, check how OSA can impact your health.
Jump over to Chapter 1: Obstructive Sleep Apnea (OSA) and its Health Effects, to delve into this fascinating subject.
And do not forget the other chapters of this guide:
- Chapter 2: Doctors Who Diagnose and Treat Obstructive Sleep Apnea.
- Chapter 3: Diagnosis of Obstructive Sleep Apnea (OSA).
- Chapter 4: Treating obstructive sleep apnea (OSA) with CPAP and dental appliances.
- Chapter 5: Treating Obstructive Sleep Apnea (OSA) with Surgery.
Enjoy!
SUTTON PLACE DENTAL ASSOCIATES ON THE WEB